Peking University team updates the 'warheads' against cancer
May 28, 2024
Editor's note: In trailblazing research, an interdisciplinary team at Peking University has made remarkable progress on targeted radionuclide therapy, adding to the arsenal against cancer – with increased potency, improved efficacy, and reduced "collateral damage."
Peking University, May 28, 2024: Prof. Liu Zhibo's team from Peking University (PKU)'s College of Chemistry and Molecular Engineering, along with collaborators, recently published a groundbreaking paper titled "Covalent targeted radioligands potentiate radionuclide therapy" in Nature. This marks the journal's first publication on radionuclide therapy since 1977. (Radionuclides are radioactive forms of elements.)
The study provides a hopeful perspective on treating metastatic cancer, which is responsible for the majority of deaths from all cancers. In 2020, cancer led to nearly 10 million deaths, accounting for one in six deaths worldwide, according to the WHO.
What is targeted radionuclide therapy (TRT)?
The Journal of Nuclear Medicine defines targeted radionuclide therapy as a (promising) treatment that "delivers ionizing radiation to tumors in a targeted manner, reducing the dose that healthy tissues are exposed to."
How does it work?
The ionizing radiation emitted by radioactive substances attached to the carrier destroys cancer cells by damaging their DNA, leading to the reduction of tumors.
What makes a successful TRT?
The efficacy of TRT can be measured by three dimensions: tumor targeting, quick blood clearance, and adequate tumor retention, as stated in the research paper.
To simplify, effective radionuclides, which act as "warheads" against cancer, need to be quickly cleared from the bloodstream to prevent toxicity. At the same time, they should remain in malignant tumors for a sufficient period to target and destroy cancer cells, considering that most therapeutic radionuclides have half-lives ranging from three to ten days. This can be a delicate balancing act.
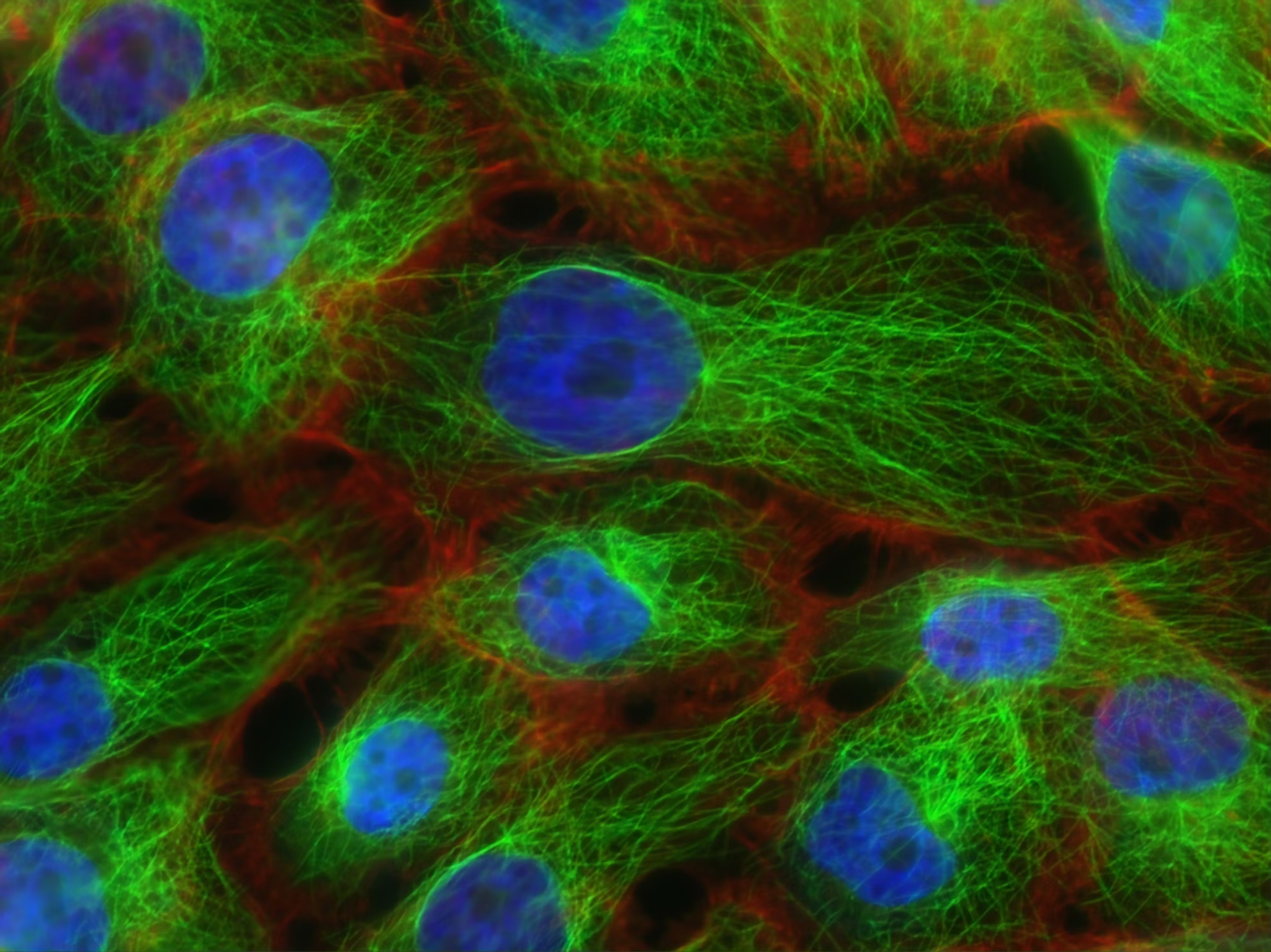
Photo/Peking University Cancer Hospital
What's new about the PKU team's method?
In the study, the PKU team incorporated a sulfur (VI) fluoride exchange (SuFEx) chemistry-based linker into radiopharmaceuticals (radioactive drugs used in cancer treatment) to enhance precise tumor targeting, quick elimination from the bloodstream, and sufficient retention in the tumor site.
Here are key takeaways from the research:
· The strategy was applied to a fibroblast activation protein (FAP) inhibitor (FAPI), resulting in over 80% covalent binding to the protein with minimal dissociation for six days. (FAP is a protein found in tumors.)
· In mice, the SuFEx-engineered FAPI showed a 257% increase in tumor uptake compared to the original FAPI, and improved tumor retention by 13 times. (Here, uptake refers to how quickly tumors absorb radiopharmaceuticals.)
· The uptake in healthy tissues was rapidly cleared.
· In a pilot imaging study, this approach detected more tumor lesions in cancer patients compared to other methods. SuFEx-engineered FAPI also effectively accomplished targeted β- and α- radionuclide therapy, leading to almost complete tumor regression in mice.
· Given the wide range of proteins that could potentially be linked to SuFEx warheads, there is a possibility of adapting this approach to target other types of cancer.
Prof. Liu Zhibo is the corresponding author of the paper, with Cui Xiyang, a researcher at Peking University, Dr. Li Zhu from Peking University Cancer Hospital, and Dr. Kong Zhiren from the National Cancer Center being the first authors.
Link to the paper: https://www.nature.com/articles/s41586-024-07461-6
Written by: Phoon Hui Yin, Andrena
Edited by: Dennis Meng
Source: College of Chemistry and Molecular Engineering
Cover photo: Unsplash